MUMBAI: A new city survey shows that many patients – almost six out of 10 – take antibiotics without medical consultation, despite research indicating that common bacteria such as E. coli have become lethal in Indian ICUs due to inappropriate use of medications. Not taking the right antibiotic in the right dosage for the right time period could result in certain bacteria developing resistance to the drug and give rise to drug-resistant infections.
A study published in ‘The Lancet’ medical journal a few months ago said that resistant bacteria, also called superbugs, could kill nearly 40 million people over the next 25 years. Antimicrobial resistance (AMR) is hence listed as one of the major public health challenges in the world.
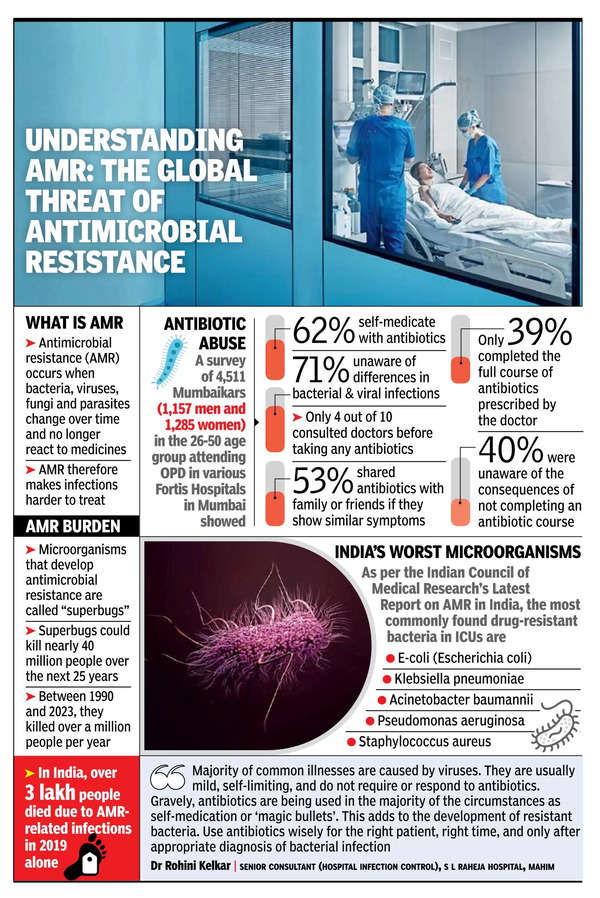
A study by the Institute for Health Metrics and Evaluation, based at the University of Washington School of Medicine, estimated that in 2019 alone, India saw nearly 3 lakh deaths attributable to AMR and another 10 lakh deaths associated with AMR. “People take antibiotics such as azithromycin and doxycycline like ‘chana-kurmura’ because their doctors prescribed it to them at some point for symptoms similar to what they have right now,” said Infectious Diseases Specialist Dr Anita Mathew from Fortis Hospital, Mulund, who was part of the team that conducted the survey.
Around 4,500 patients and their relatives visiting four Fortis Hospitals in the city were surveyed about their attitude towards antibiotics; 62% said they self-prescribed antibiotics when they had a common cold, throat pain, or flu. “Antibiotics are not a one-size-fits-all solution; they need to be tailored based on the infection site and the bacteria we suspect. For conditions such as the flu, which is caused by a virus and not bacteria, antibiotics are not effective. Since flu is self-limiting, it typically resolves on its own without the need for antibiotics,” added Dr Mathew.
Her colleague from the Kalyan hospital, Dr Kirti Sabnis, said that around 71% of those surveyed were unaware of the differences between bacterial and viral infections. Antibiotics are used to treat bacterial infections, while antivirals and antifungals are used to treat viral and fungal infections respectively; misusing or wrongly using any of these medicines could contribute to the corresponding microbe becoming drug-resistant and emerging as superbugs.
According to Professor Dr Mala Kaneria from BMC-run Nair Hospital near Mumbai Central railway station, the levels of antimicrobial resistance in the country are highly worrisome. “We are now encountering patients with pan drug resistance as opposed to multidrug resistance, with none of the known antibiotics working for them,” she said. Doctors have to work out or repurpose other drugs to save lives in ICU. “There must be no ICU in the country without a case of pan or multi-drug-resistance,” she said.
Until 20 years ago, many bacteria could be treated with the drugs specifically designed for them. “Pseudomonas aeruginosa has become a real cause for worry now, and Staphylococcus aureus has emerged as MRSA that is no longer easy to treat,” added Dr Kaneria.
The annual AMR report by the Indian Council of Medical Research said that diseases such as urinary tract infections, pneumonia, and typhoid have developed resistance to commonly used antibiotics. Analysing almost 1 lakh samples from over 200 hospitals across the country, the ICMR report found that the susceptibility of E. coli, the most common bacteria across OPDs and ICUs, to many antibiotics dropped by 10% to 20% between 2017 and 2023. The susceptibility of Klebsiella pneumoniae and Pseudomonas aeruginosa to antibiotics such as imipenem and meropenem has dropped in the same period.
Dr Mathew said a patient in her eighties who was getting admitted with frequent infections passed away on Friday due to sepsis. “As she was recently admitted for a urinary tract infection, we started her on high-end antibiotics right away this time around. We even put her on colistin, the last-resort antibiotic, but she succumbed,” said the doctor. Dr Sabnis said that people’s awareness and attitude have to change so that today’s antibiotics are still effective for future generations. “The problem is people look for quick fixes. They have a viral infection that would take a week to resolve, but they presume their body is a machine that can heal faster without rest. Even patients with diabetes want their infections to resolve within a day or two without realising that recovery could be longer for those with no baseline fitness,” she added.